Sciatica is common, affecting 10% to 40% of the population.1 Despite it being commonplace, many myths and misconceptions persist and, in turn, make it hard for people with sciatica to get better.
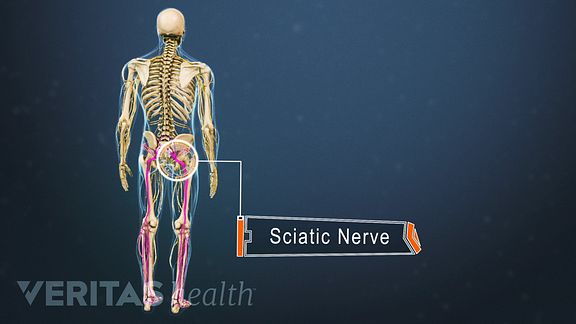
Sciatica arises when a part of the sciatic nerve is pinched or irritated.
Watch: Sciatica Causes and Symptoms Video
Here are 10 definitive facts about sciatica to quickly get you up to speed:
1. Sciatica overlaps with multiple diagnoses
The medical term for sciatica is lumbar radiculopathy. It can also be described as pinched or compressed nerve pain (originating in your lower spine). Some doctors may refer to the underlying condition causing your sciatica, such as a herniated disc or spinal stenosis (narrowing of bony openings for nerves or the spinal cord).
See Sciatica Causes
It may be confusing if you hear these terms used together or interchangeably, but don’t worry—it doesn’t necessarily mean that you have 4 or 5 different diagnoses.
2. Sciatica refers to a set of symptoms
Sciatica is defined by a number of symptoms caused by an underlying medical condition; it is not a medical diagnosis.2 Leg pain is typically noted as the most bothersome symptom of sciatica.3 You may also feel numbness, tingling, and/or weakness, typically affecting one leg at a time.1
3. Level of spinal nerve involvement matters
Depending on the nerve root affected, the symptoms of sciatica can vary. For example, symptoms from the S1 nerve root in your lower spine may cause marked pain along the back of your thigh, leg, and/or the outer side of your foot, but the L5 nerve typically causes weakness in the foot.4
It is possible for more than one nerve root to be affected at a time, causing overlapping symptoms. Depending on the spinal level affected, sciatica can be lumbar, sacral, or lumbosacral radiculopathy.
4. The risk increases with height and weight
If you are tall and/or overweight, you may be at a higher risk of developing sciatica. This risk increases with age1 and is more common among men who are above 185 cm (6 ft 1 in) in height.5
People who are overweight and have sciatica due to disc herniation may also be at a higher risk of hospitalization and/or surgery for their sciatica pain.6
See Weight Loss for Back Pain Relief
In This Article:
- Is My Pain Sciatica or Something Else?
- 10 Quick Facts About Sciatica
- 4 Commonly Overlooked Sciatica Remedies
- Is Surgery the Quickest Path to Sciatica Relief?
5. Treatment depends on the cause
Sciatica is typically caused by a problem in your lower back, such as herniated or degenerated discs, spinal stenosis, or spondylolisthesis (slipping of a vertebra over the one below it), to name a few.1
See Diagnosing the Cause of Sciatica
To treat sciatica, it is essential to obtain an accurate diagnosis of the underlying cause, since the treatment of each condition may be unique and different from the others.
6. Usually, there is good response to treatment
Sciatica usually responds well to medical treatment without long-term complications. Your pain may even resolve without any treatment. Typically, relief is seen in 4 to 6 weeks.1 When progressive neurological symptoms, such as severe weakness and/or numbness is present, minimally invasive treatments or surgery may be suggested.
See Myths About Sciatica Treatment Options
7. Medical emergencies are possible
Rarely, certain sciatica symptoms may require immediate treatment, including but not limited to:
- Worsening neurological symptoms, such as numbness and/or weakness
- Symptoms in both legs
- Bladder and/or bowel incontinence
- Numbness in the genital or groin areas
These symptoms may indicate serious underlying conditions, such as spinal nerve damage, spinal cord damage, or cauda equina syndrome. As a general rule, see a doctor for any concerning or worsening symptoms.
See When Sciatica Pain Is a Medical Emergency
8. Long-term results of surgical and nonsurgical treatments are usually similar
Sciatica surgery may provide immediate pain relief, with results sustaining up to 1 year. But research suggests that after 4 to 10 years, the effectiveness of surgical and nonsurgical treatments is usually the same.7,8
See Sciatica Surgery
9. Other conditions can mimic sciatica
If you have a pelvic muscle spasm (piriformis syndrome), broken hip bone, arthritic hip joint (hip osteoarthritis), or the dysfunction of a joint in the pelvis (sacroiliac joint dysfunction or inflammation) the pain may feel similar to sciatica.
Degeneration or compression of the body of the sciatic nerve or its branches in the leg can also mimic sciatica pain.
See Causes of Leg Pain and Foot Pain
10. Exercise is better than rest
While bed rest may seem like a good option to relieve your sciatica, experts recommend following a structured exercise routine to keep the symptoms at bay.9,10 Exercise can help nourish your spinal discs, improve muscle and bone strength, and improve the flexibility of your sciatic nerve—for both immediate and long term benefits.
It is important that you learn sciatica exercises from a trained medical professional to ensure correct posture and technique and avoid other injuries or complications.
See Sciatica Exercises for Sciatica Pain Relief
If you have sciatica, consult your doctor for a diagnosis of the underlying problem. Prompt diagnosis and treatment can help control the pain and prevent the progression of symptoms.
Learn more:
Watch Sciatica Treatment Video
Referrence
- 1.Davis D, Vasudevan A. Sciatica. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/.
- 2.Cook CE, Taylor J, Wright A, Milosavljevic S, Goode A, Whitford M. Risk Factors for First Time Incidence Sciatica: A Systematic Review. Physiotherapy Research International. 2013;19(2):65-78. doi:10.1002/pri.1572.
- 3.Grøvle L, Haugen AJ, Natvig B, Brox JI, Grotle M. The prognosis of self-reported paresthesia and weakness in disc-related sciatica. Eur Spine J. 2013;22(11):2488–2495. doi:10.1007/s00586-013-2871-9
- 4.Wright R, Inbody SB. Radiculopathy and Degenerative Spine Disease. In: Neurology Secrets. Elsevier; 2010:121-130. doi:10.1016/b978-0-323-05712-7.00007-6.
- 5.Heuch I, Heuch I, Hagen K, Zwart JA. Association between body height and chronic low back pain: a follow-up in the Nord-Trøndelag Health Study [published correction appears in BMJ Open. 2015;5(10):e006983]. BMJ Open. 2015;5(6):e006983. Published 2015 Jun 15. doi:10.1136/bmjopen-2014-006983
- 6.Shiri R, Lallukka T, Karppinen J, Viikari-Juntura E. Obesity as a Risk Factor for Sciatica: A Meta-Analysis. American Journal of Epidemiology. 2014;179(8):929-937. doi:10.1093/aje/kwu007
- 7.Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2.
- 8.Gugliotta M, da Costa BR, Dabis E, et al. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open. 2016;6(12):e012938. Published 2016 Dec 21. doi:10.1136/bmjopen-2016-012938
- 9.Koes B. Moderate quality evidence that compared to advice to rest in bed, advice to remain active provides small improvements in pain and functional status in people with acute low back pain. Evidence-Based Medicine. 2010;15(6):171-172. doi:10.1136/ebm1132
- 10.Fernandez M, Hartvigsen J, Ferreira ML, et al. Advice to Stay Active or Structured Exercise in the Management of Sciatica. Spine. 2015;40(18):1457-1466. doi:10.1097/brs.0000000000001036